Age related cataract may initially be corrected to some extent by spectacles but surgery is the only cure. Cataract surgery is not only one of the most commonly performed surgical procedure in the world but is also the surgery with one of the highest success rates. It is low risk, fast and highly effective. However, the longer you wait to have cataract surgery, the most likely is that you can experience some setbacks. It is important to get a correct diagnosis and advise regarding cataract and the timing of surgery.
At Nayana Eye Care, you get a comprehensive eye examination which is necessary to assess the cataract and our highly qualified and experienced surgeons will guide you to get the best possible visual outcome with the latest techniques and technology.
Techniques:
Phacoemulsification
This technology uses ultrasound energy to break the cataract in to multiple small pieces inside the eye so that they can be removed through a very small incision (2.8 mm). This is the preferred technique to deal with cataracts worldwide. The advantages are
- It doesn’t produce a scar
- It doesn’t require a stitch
- It is a totally bloodless surgery and is safe to perform on people using blood thinners for heart conditions
- Surgery is done inside a closed chamber
- A very small incision leads to minimal or no post-operative astigmatism reducing the dependency on glasses for distance vision
- Patient will have a choice to choose modern IOLs to get the desired visual outcome
MICS
Micro incision cataract surgery is a term often used if phacoemulsification is performed in a 2.2 mm incision. Modern foldable IOLs can be implanted in to the eye with incisions as small as 2.2 mm, resulting in negligible post-operative astigmatism and exception visual outcomes.
SICS
Small incision cataract surgery or SICS is a technique which doesn’t require use of any automated machinery. It is a manual procedure where the cataract is delivered outside the eye as a whole without breaking it in to smaller pieces. It requires an incison size of 6 mm or larger and is widely performed, especially in advanced mature cataracts or complicated cataracts. It produces
Choices of IOLs
In today’s era the ageing population continues to work, stay active later in life. Therefore their need for quality vision at both distance and near is also growing. The cataract surgery has transitioned from restoring vision to offering spectacle independence.
Types of vision needed in daily life
- Distance vision: Watching TV, reading subtitles, reading sign boards, driving
- Near vision: Reading newspaper and books, reading on mobile devices or tablets, doing needle or craft work, reading price tags
- Intermediate vision: Working on computers or laptops, cooking, eating, playing chess or cards, using stairs or walking on uneven surfaces
Monofocal IOLs :
The most common type of lens used with cataract surgery is called a monofocal IOL. It has one focusing distance. It is set to focus for distance vision. Those who opt for these lenses have good distance vision but will have to wear eyeglasses for near and intermediate vision.
Bifocal IOLs:
Bifocal IOLs have different zones on their surface that will help to provide good vision for both distance and near. They may need glasses to view intermediate vision clearly.
Trifocal IOLs
Trifocal IOLs can offer spectacle independence for distance, near and intermediate vision.
Toric IOLs
For people with astigmatism, there is an IOL called Toric IOL. Astigmatism is a refractive error caused by an uneven curve on the cornea. The toric IOL is designed to correct that irregularity on the cornea so that post-operatively glasses would not be required. Toric IOLs are available in all the three above segments (Monofocal, Bifocal and Trifocal).

cornea clinic
Our corneal surgeon is highly experienced in treating various corneal conditions that include anterior segment trauma, ocular surface diseases including dry eye, contact lens related eye conditions, microbial keratitis management and refractive surgery.
Investigations
Corneal topography (Pentacam)
Corneal topography is a technology that creates 3D maps of the surface curvature of the cornea. Corneal topography produces a detailed, visual description of the shape and power of the cornea. This analysis provides your doctor with very fine details of the cornea used to diagnose, monitor, and treat various eye conditions. They are also used in fitting contact lenses and for planning surgery, including laser vision correction like PRK and LASIK.
Specular microscopy
It is a technology used to assess the morphology, density and function of corneal endothelial cells. Endothelium is the innermost of the 5 layers of cornea.
Common ocular conditions, such as glaucoma, uveitis and Fuchs endothelial dystrophy, may produce changes in the structure and function of the corneal endothelium that result in corneal edema and visual impairment. Additionally, clinical circumstances, such as contact lens wear and intraocular surgery, may compromise the endothelium and cause corneal edema. An accurate diagnosis of endothelial disease may be the key in not only determining cause of corneal edema, but also developing a treatment plan.
Corneal surgical procedures
Pterygium surgery:
Pterygium surgery is a procedure performed to remove the conjunctival growth on the cornea. A pterygium is a growth of scar-like tissue of the conjunctiva onto the edge of the cornea. It typically occurs on the nose side of the eye but can also occur on the ear side. Small pterygia are common and often don’t cause significant symptoms. They can cause redness and irritation. If they get large, they can also affect the vision. If they cause decreased vision or severe discomfort, they can be surgically removed.
The pterygium is excised and some conjunctival tissue from the upper part of the eye is removed and placed in the area from which the pterygium was removed, to decrease the chance of recurrence of the pterygium. However, the pterygium can occasionally recur. Pterygium surgery is performed using local or topical anesthesia.
Corneal Collagen cross linking:
Corneal collagen cross-linking or C3R is a treatment for an eye problem called Keratoconus In this condition, the front part of your eye, called the cornea, thins out and gets weaker over time. This makes it bulge into a cone shape, which can distort your vision and make it hard to see. If the symptoms of keratoconus get severe, you will need a corneal transplant. In corneal cross-linking, doctors use eyedrop medication and ultraviolet (UV) light from a special machine to make the tissues in your cornea stronger. The goal is to keep the cornea from bulging more. It’s called “cross-linking” because it adds bonds between the collagen fibers in your eye. They work like support beams to help the cornea stay stable. Corneal cross-linking is the only treatment that can stop progressive keratoconus from getting worse. And it may help you avoid a corneal transplant, which is major surgery.
Retina services:
Age, diabetes, hypertension, myopia and trauma are a few conditions that can predispose an eye to retinal disease. It is very important to visit a retina specialist immediately if you notice sudden loss of vision, reddish hue in vision, sudden appearance of dark spots or threads or insect like objects moving in your visual field or wavy or distorted vision to name a few.
Investigations
Fundus fluorescein angiography (FFA)
This investigative procedure comprises of injecting a dye called fluorescein into one of the veins in your arm and taking rapid serial photographs of its passage within the delicate blood vessels of the eye in the retina and choroid, using a digital Fundus camera.
The information obtained from this test aids your doctor in making a diagnosis and planning treatment like laser or intravitreal injections.
Apart from the needle prick and the light flash of the camera there is no discomfort from this test. A few patients may have nausea and by remaining calm and taking deep breaths help overcome it. Your usual diet can be taken soon after the procedure. Fluorescein is a non-toxic drug. In rare instances, it can produce an allergic reaction, which responds rapidly to appropriate medication. Serious life-threatening allergic reactions, though exceptionally rare, can occur. The skin and urine may appear yellow in colour for about 36 hours following the test and is not a cause of any concern.
You must be accompanied by an adult attendant during this test.
Optical coherence tomography (OCT)
It is a non-invasive, non-contact imaging technology, with ultra-high speed 27,000 axial scans per second. It provides high-resolution 5-µm axial and 15-µm transverse resolution in tissue.
The procedure requires you to sit in front of the OCT machine and place your chin on chin rest and forehead touching the head support. You are required to focus at a given target and keep your eye still while the scan is being performed.
The layers within the retina can be differentiated and the retinal thickness can be measured. Also, the change from the previous visit, the effect of treatment can be analyzed.
B-scan
B SCAN is a two-dimensional imaging system which utilizes high-frequency sound waves ranging from 8-10 MHz. It is used for imaging of intraocular structures and giving information about the status of the lens, vitreous, retina, choroid, and sclera.
B-scan ultrasound is most useful when direct visualization of intraocular structures is difficult or impossible in cases like corneal opacities, miosis, pupillary membranes, dense cataracts, or vitreous opacities.
In many instances, ultrasound is used for diagnostic purposes even though pathology is clinically visible. Such instances include differentiating intraocular tumors, rhegmatogenous versus exudative retinal detachments, and disc drusen versus papilledema.
Retinal treatment procedures:
Intravitreal Anti-VEGF injections:Intravitreal Anti-VEGF injections are the first line of therapy in a variety of retinal conditions like diabetic macular edema, cystoid macular edema in vascular occlusions, wet age related macular degeneration, polypoidal choroidal vasculopathy etc.
Intravitreal steroid injections:They are used to treat uveitic cystoid macular edema, recurrent or macular edema not responding to anti-VEGF injections.
Retinal lasers:
Pan retinal photocoagulation: This usually involves multiple sessions spaced 10-15 days apart and are used to treat conditions like proliferative diabetic retinopathy, vein occlusions etc.
Focal laser: This is usually a single session and a short procedure used to treat conditions like central serous retinopathy, diabetic macular edema etc
Retinal surgeries:
Retinal surgeries are carried out to treat certain conditions like retinal detachments, epiretinal membranes, macular holes, vitreous hemorrhage and others.
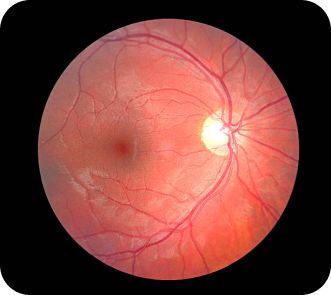
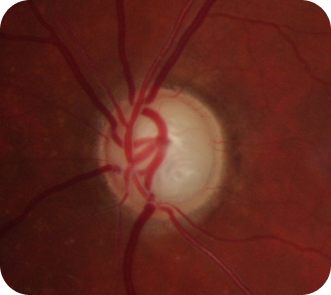
Glaucoma
The increased pressure in your eye, can damage your optic nerve, which sends images to your brain. If the damage worsens, glaucoma can cause permanent loss of vision or even total blindness within a few years.
Most people with glaucoma have no early symptoms or pain. Visit your eye doctor regularly so they can diagnose and treat glaucoma before you have long-term vision loss.
If you lose vision, it can’t be brought back. But lowering eye pressure can help you keep the sight you have. Most people with glaucoma who follow their treatment plan and have regular eye exams are able to keep their vision.
You’re more likely to get it if you:
- Are over 40 years old
- Have a family history of glaucoma
- Are nearsighted or farsighted
- Have poor vision
- Have diabetes
- Take certain steroid medications such as prednisolone
- Have had an injury to your eye or eyes
- Have corneas that are thinner than usual
- Have high blood pressure, heart disease, diabetes, or sickle cell anemia
- Have high eye pressure
Types of glaucoma
There are two main kinds:
Open-angle glaucoma: This is the most common type. Your doctor may also call it wide-angle glaucoma. The drain structure in your eye (called the trabecular meshwork) looks fine, but fluid doesn’t flow out like it should.
Angle-closure glaucoma: This is more common in Asia. You may also hear it called acute or chronic angle-closure or narrow-angle glaucoma. Your eye doesn’t drain like it should because the drain space between your iris and cornea becomes too narrow. This can cause a sudden increase of pressure in your eye. It’s also linked to farsightedness and cataracts.
Less common types of glaucoma include:
Secondary glaucoma: This is when another condition, like cataracts or diabetes, causes added pressure in your eye.
Normal-tension glaucoma: This is when you have blind spots in your vision or your optic nerve is damaged even though your eye pressure is within the average range. Some experts say it’s a form of open-angle glaucoma.
Pigmentary glaucoma: With this form, tiny bits of pigment from your iris, the coloured part of your eye, get into the fluid inside your eye and clog the drainage canals.
Symptoms
Most people with open-angle glaucoma don’t have symptoms. If symptoms do develop, it’s usually late in the disease. That’s why glaucoma is often called the "silent thief of vision." The main sign is usually a loss of side, or peripheral, vision.
Symptoms of angle-closure glaucoma usually come on faster and are more obvious. Damage can happen quickly. If you have any of these symptoms, get medical care right away:
- Seeing halos around lights
- Vision loss
- Redness in your eye
- Eye that looks hazy (particularly in infants)
- Upset stomach or vomiting
- Eye pain
Diagnosis
Glaucoma tests are painless and don’t take long. Your eye doctor will test your vision. They’ll use drops to widen (dilate) your pupils and examine your eyes. They’ll check your optic nerve for signs of glaucoma. They may take photographs so they can spot changes at your next visit. They’ll do a test called tonometry to check your eye pressure. They may also do a visual field test to see if you've lost peripheral vision. If your doctor suspects glaucoma, they may order special imaging tests of your optic nerve.
Treatment:
Your doctor may use prescription eye drops, oral medications, laser surgery, or microsurgery to lower pressure in your eye.
Eye drops: These either lower the creation of fluid in your eye or increase its flow out, lowering eye pressure. Side effects can include allergies, redness, stinging, blurred vision, and irritated eyes. Some glaucoma drugs may affect your heart and lungs. Because of potential drug interactions be sure to tell your doctor about any other medical problems you have or other medications you take. Also let them know if it’s hard for you to follow a regimen involving two or three different eye drops or if they have side effects. They may be able to change your treatment.
Oral medication: Your doctor might also prescribe medication for you to take by mouth, such as a beta-blocker or a carbonic anhydrase inhibitor. These drugs can improve drainage or slow the creation of fluid in your eye.
- IridotomyThis makes a tiny hole in your iris to let fluid flow more freely.
Microsurgery: In a procedure called a trabeculectomy, your doctor creates a new channel to drain the fluid and ease eye pressure. Sometimes an a valve or an implant may be required in addition to trabeculectomy.
Open-angle glaucoma is most often treated with combinations of eye drops, laser trabeculoplasty, and microsurgery. Doctors tend to start with medications, but early laser surgery or microsurgery could work better for some people.
Acute angle-closure glaucoma is usually treated with a laser procedure.
